PTSD e Depressione: Comprendere la Sovrapposizione e Come un Test PTSD Gratuito Chiarire i Sintomi
November 11, 2025 | By Henry Davis
Sentirsi persi in una nebbia di emozioni difficili è un peso gravoso da portare. Potresti essere alle prese con una tristezza persistente, un senso di intorpidimento o ricordi intrusivi che disturbano la tua vita quotidiana. È comune chiedersi cosa stia realmente accadendo. È trauma? È depressione? La confusione è comprensibile, poiché i sintomi del Disturbo da Stress Post-Traumatico (PTSD) e della depressione possono spesso apparire e sentirsi notevolmente simili. Molte persone si chiedono: ho il PTSD o sono solo traumatizzato?

Questa guida è qui per offrire chiarezza. Esploreremo i sintomi condivisi, scopriremo le differenze chiave e spiegheremo come una valutazione strutturata possa essere un potente primo passo verso la comprensione delle tue esperienze. Prendersi un momento per l'auto-riflessione può illuminare il percorso, e un test di screening del PTSD online fornisce un punto di partenza confidenziale per quel viaggio.
Comprendere i Sintomi del PTSD e della Depressione
A prima vista, il PTSD e il Disturbo Depressivo Maggiore (MDD) condividono un terreno emotivo significativo. Entrambe le condizioni possono lasciarti con un senso di disconnessione dagli altri, esausto e in difficoltà a trovare gioia nelle attività che un tempo amavi. Questa sovrapposizione non è solo una coincidenza; è radicata nel modo in cui il nostro cervello elabora lo stress travolgente e il dolore emotivo. Comprendere queste lotte condivise è il primo passo per districarle.
Lotte Comuni: Intorpidimento Emotivo, Anedonia e Altro
Una delle sovrapposizioni più confuse è la sensazione di essere emotivamente distaccati. Questo intorpidimento emotivo può fungere da meccanismo di difesa, un modo per la mente di proteggersi dal dolore travolgente. Può sembrare che si stia semplicemente andando avanti per inerzia, distaccati dalla propria vita.
Un altro filo conduttore comune è l'anedonia, un termine che gli psicologi usano per la perdita di piacere o interesse nelle attività che un tempo ti procuravano gioia. Hobby, amicizie e persino cibi preferiti possono perdere il loro fascino. Questo è spesso accompagnato da ritiro sociale, alterazioni negative dell'umore, disturbi del sonno (troppo o troppo poco) e difficoltà di concentrazione. Per chi sperimenta questi sintomi, distinguere la causa principale può sembrare impossibile.
La Risposta del Cervello: Come il Trauma Influisce sulla Regolazione dell'Umore
Perché queste condizioni si sovrappongono così tanto? La risposta risiede nella nostra neurobiologia. Un evento traumatico può disregolare il sistema di risposta allo stress del corpo, influenzando le parti del cervello responsabili della regolazione dell'umore, della memoria e dell'elaborazione delle emozioni. L'amigdala (il "centro della paura" del cervello) può diventare iperattiva, mentre la corteccia prefrontale (responsabile del ragionamento e del controllo) può diventare meno efficace.
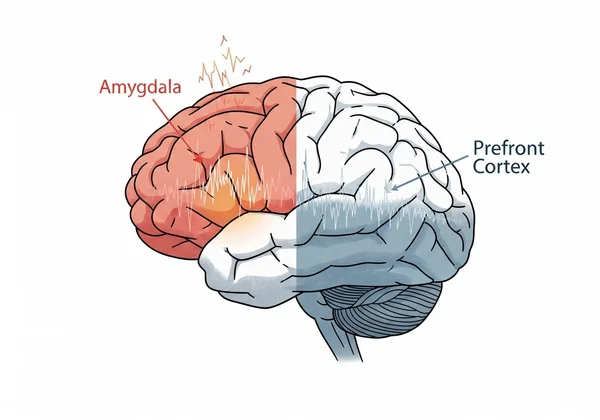
Questa interruzione può portare direttamente ai sintomi di iperattivazione osservati nel PTSD, come essere facilmente spaventati o costantemente in allerta. Allo stesso tempo, lo stress prolungato e il tributo emotivo possono esaurire neurotrasmettitori come la serotonina e la dopamina, cruciali per mantenere un umore stabile, contribuendo ai persistenti sentimenti di malessere caratteristici della depressione. Il trauma può essere una via diretta alla depressione, o i due possono svilupparsi contemporaneamente, creando un quadro clinico complesso.
Distinguere tra PTSD e Disturbo Depressivo Maggiore
Anche se le conseguenze emotive possono sembrare simili, il PTSD e la depressione sono condizioni distinte con marcatori diagnostici unici. Identificare queste differenze è cruciale per cercare il giusto tipo di supporto. Mentre la depressione è principalmente un disturbo dell'umore, il PTSD è un disturbo correlato a traumi e stress, il che significa che i suoi sintomi sono direttamente collegati a un evento traumatico specifico o a una serie di eventi traumatici. Un test PTSD online confidenziale è progettato per lo screening di questi marcatori specifici.
Marcatori Unici del PTSD: Intrusioni, Evitamento e Iperattivazione
Le caratteristiche fondamentali che distinguono il PTSD sono direttamente legate al ricordo traumatico. Questi sono spesso raggruppati in quattro categorie di sintomi:
- Sintomi di intrusione: Questo è forse l'aspetto più noto del PTSD. Include ricordi indesiderati e angoscianti, flashback in cui ci si sente come se si stesse rivivendo l'evento e incubi relativi al trauma. Questi sintomi di intrusione non sono solo ricordi tristi; sono rivissuti vividi e involontari.
- Evitamento: Una persona con PTSD farà di tutto per evitare i richiami del trauma. Questo può significare evitare persone, luoghi, conversazioni o attività che scatenano ricordi o sentimenti angoscianti. Questo schema di evitamento è uno sforzo deliberato per tenere a bada il trauma.
- Alterazioni negative della cognizione e dell'umore: Questo assomiglia molto alla depressione ma è radicato nel trauma. Include credenze negative persistenti su se stessi o sul mondo (ad es., "Sono cattivo", "Il mondo è pericoloso"), colpa distorta e incapacità di provare emozioni positive.
- Iperattivazione: Questo implica essere in uno stato costante di alta allerta. I sintomi includono irritabilità, scoppi d'ira, comportamento spericolato, essere facilmente spaventati e problemi di concentrazione e sonno. Questo stato di iperattivazione riflette un sistema nervoso bloccato in modalità "lotta o fuga".
Caratteristiche Fondamentali della Depressione: Tristezza Persistente e Perdita di Spinta
Al contrario, le caratteristiche fondamentali del Disturbo Depressivo Maggiore non sono necessariamente collegate a un ricordo intrusivo specifico. Mentre il trauma può essere un fattore scatenante per la depressione, i sintomi possono anche manifestarsi senza un evento esterno identificabile. Le caratteristiche distintive della depressione sono:
- Tristezza Persistente: Un umore basso pervasivo o un senso di vuoto presente per la maggior parte del giorno, quasi ogni giorno.
- Perdita di Spinta: Questa è una profonda perdita di interesse o piacere in tutte le attività, o quasi tutte: il termine clinico è anedonia. È più che semplice noia; è una profonda mancanza di motivazione e divertimento.
Altri sintomi chiave includono cambiamenti significativi di peso, disturbi del sonno, affaticamento o perdita di energia, sentimenti di inutilità o eccessiva colpa e pensieri ricorrenti di morte o suicidio. Mentre una persona con PTSD può sperimentare questi sintomi, nel MDD essi costituiscono la lotta centrale senza la necessità di flashback intrusivi specifici del trauma o comportamenti di evitamento. Comprendere il tuo schema unico è il primo passo, e un test di autovalutazione del PTSD può aiutare.
Come un Test PTSD Può Chiarire il Tuo Profilo Sintomatologico
Navigare questo complesso panorama emotivo da soli può essere scoraggiante. È qui che uno strumento di valutazione strutturato fornisce un valore immenso. Un test di screening del PTSD ben progettato agisce come uno specchio, riflettendo le tue esperienze in modo organizzato. Ti aiuta a passare da una vaga sensazione di "qualcosa non va" a un quadro più chiaro delle tue sfide specifiche.
Il Ruolo degli Strumenti di Screening Standardizzati (es. PCL-5)
I test online affidabili non sono quiz casuali. Il nostro test si basa sul PCL-5 (PTSD Checklist for DSM-5), lo stesso standard utilizzato da clinici e ricercatori in tutto il mondo. Questo strumento consiste in un elenco di domande che corrispondono direttamente ai criteri diagnostici ufficiali del PTSD. Chiedendoti di valutare quanto sei stato infastidito da sintomi specifici nell'ultimo mese, valuta sistematicamente la presenza di sintomi di intrusione, evitamento e iperattivazione che sono unici del PTSD. Questo approccio strutturato aiuta a quantificare le tue esperienze, rendendo più facile vedere se il tuo profilo sintomatologico si allinea più strettamente con il PTSD.
Ottenere Approfondimenti Iniziali per Conversazioni Professionali
È fondamentale ricordare che un test online è uno strumento di screening, non una diagnosi. Una diagnosi formale può essere fatta solo da un professionista della salute mentale qualificato. Tuttavia, i risultati di un test confidenziale possono essere un punto di partenza inestimabile.
Invece di andare da un medico e dire: "Mi sento malissimo", puoi presentarti con informazioni specifiche: "Ho fatto uno screening basato sul PCL-5 e i miei risultati suggeriscono che sto sperimentando significativi ricordi intrusivi e comportamenti di evitamento". Questo ti permette di avere una conversazione più mirata e produttiva con i professionisti sanitari. Ti fornisce il linguaggio per descrivere il tuo mondo interiore e offre loro un quadro più chiaro fin dal primo appuntamento. Fare un test PTSD gratuito è un passo proattivo, privato e potente verso la ricerca del giusto aiuto.
Il Tuo Primo Passo Verso la Chiarezza e il Supporto Mirato
Sentirsi confusi da sintomi sovrapposti di trauma e tristezza non è un segno di debolezza; è un segno che stai cercando di dare un senso a un'esperienza difficile. Comprendere le differenze chiave tra PTSD e depressione è il primo passo verso la ricerca del giusto percorso di guarigione. Mentre entrambi comportano un profondo dolore emotivo, il PTSD è definito in modo unico dal suo legame diretto con un ricordo traumatico attraverso intrusioni, evitamento e iperattivazione.
Non devi affrontare questa incertezza da solo. Ottenere chiarezza è possibile, e inizia con un singolo, coraggioso passo. Utilizzando uno strumento confidenziale e basato sulla scienza, puoi ottenere preziose intuizioni sui tuoi sintomi e sentirti più preparato a cercare una guida professionale.
Pronto a fare quel primo passo? Fai il nostro test PTSD gratuito oggi per esplorare in modo confidenziale i tuoi sintomi e muoverti verso un futuro con maggiore comprensione e speranza.
Domande Frequenti su PTSD e Depressione
Ho il PTSD o ansia?
Questo è un altro punto comune di confusione. Entrambi comportano un'intensa preoccupazione e sintomi fisici di eccitazione. Tuttavia, il focus della paura è diverso. Il Disturbo d'Ansia Generalizzato (GAD) spesso comporta una preoccupazione persistente per vari aspetti della vita, come il lavoro, la salute o la famiglia. Nel PTSD, l'ansia e l'iperattivazione sono specificamente legate ai richiami di un evento traumatico.
Cosa succede se il PTSD non viene trattato?
Se non trattati, i sintomi del PTSD possono diventare cronici e influenzare gravemente tutte le aree della vita, comprese le relazioni, la carriera e la salute fisica. Può aumentare il rischio di sviluppare altre condizioni come depressione, disturbi da uso di sostanze e altri disturbi d'ansia. Cercare supporto è un passo fondamentale per prevenire complicazioni a lungo termine.
Il PTSD può scomparire?
Con un trattamento efficace, le persone possono recuperare dal PTSD. Terapie come la Terapia Cognitivo Comportamentale (CBT) e la Desensibilizzazione e Rielaborazione tramite Movimenti Oculari (EMDR) sono altamente efficaci. Anche se i ricordi dell'evento rimarranno, il trattamento può ridurre o eliminare significativamente i sintomi angoscianti, permettendoti di riprendere il controllo della tua vita.
Quanto sono accurati i test PTSD online?
L'accuratezza di un test online dipende interamente dal suo design. Un test basato su una misura clinicamente validata come il PCL-5, come la valutazione PTSD online offerta qui, può essere uno strumento di screening altamente affidabile. Fornisce una forte indicazione se i tuoi sintomi giustificano un'ulteriore valutazione da parte di un professionista, fungendo da primo passo accurato.
Cosa fare dopo un test PTSD?
Dopo aver fatto un test, prenditi un momento per rivedere i tuoi risultati. Usali come strumento per l'auto-riflessione. Il passo successivo più importante è condividere questi risultati con un operatore sanitario di fiducia, come un medico o un professionista della salute mentale abilitato. Possono condurre una valutazione completa, fornire una diagnosi formale e discutere le opzioni di trattamento più efficaci per te.